The Ultimate Guide to Vitamin D and Polycystic Kidney Disease
May 17, 2023In the United States, an estimated 42% of adults have a Vitamin D deficiency.(1) Worldwide, deficiency is even more prevalent with estimates of over 50% of the world’s population as being deficient in Vitamin D.(2)
That percentage jumps way up to 80% when looking at individuals with impaired kidney function, including CKD and PKD.(3, 4)
I am finding, as a Registered Dietitian and specialist in PKD, that a Vitamin D deficiency is quite common with PKD, no matter how young or old you are!
Before we get into PKD and vitamin D, I want to give you a little background on, and an introduction to, Vitamin D.
What is Vitamin D?
Vitamin D is a fat-soluble vitamin. This means exactly what it sounds like. Vitamin D dissolves in fat and is better absorbed better, in the gut, when there is some fat present. It's not surprising that body Vitamin D is stored primarily in our fatty tissue.(5)
In the body, Vitamin D helps to promote the absorption of calcium. Calcium is a key component of bone health, and Vitamin D helps maintain the balance between calcium and phosphorus. This balance is key to keeping bones strong and healthy. Together with calcium, Vitamin D helps prevent brittle bones and osteoporosis.
But that's not it, Vitamin D is part of many important biological functions in the body and plays an important role in multiple biological pathways. There are vitamin D receptors all over the body!
Vitamin D plays a role in immune function, cell growth, hormone production, and regulation of the inflammation process.(6) Your Vitamin D intake, and status, are also important for kidney health with Polycystic Kidney Disease.
Research shows that Vitamin D helps:
-
Bone health (7)
-
Reduce the risk of some cancer risks (10)
-
Supports better blood sugar regulation and prevention of Type II DM (11)
-
Immune system regulation (12)
Sources of Vitamin D
There are three main ways to get Vitamin D. It can be made in the body, you can get it through diet, and with supplements.
Produced in the Body
Your body makes vitamin D naturally, from cholesterol, when it's exposed to sunlight (UVB rays). That's how it got nicknamed “the sunshine vitamin”. Things that can decrease the production of vitamin D are older age, darker skin pigmentation, limited sun exposure, sunscreen, and even smog.(13)
Naturally Occurring
Vitamin D is only in a handful of foods naturally, primarily from animal sources. Naturally occurring sources include fatty fish, some cheeses, egg yolks, and some mushrooms.
Although fatty fish is a good source of Vitamin D, you would have to eat it almost daily to meet your intake needs. Examples of fatty fish include salmon, rainbow trout, tuna, and mackerel.
Vitamin D content examples:
-
3 oz salmon contains around 570 IU
-
3 oz of canned tuna contains around 190 IU
-
Fish Oil: cod liver oil, 1 teaspoon contains about 400 IU
*includes high levels of Vitamin A
In comparison, a few other natural sources of Vitamin D:
-
Eggs Yolks, 1 yolk contains 44 IU
-
Certain mushrooms, like portobello mushrooms, also contain Vitamin D. However, this is a pretty small amount.

Source: USDA FoodData Central
Fortified Foods
Most Americans’ primary intake comes from foods fortified with Vitamin D.(14, 15) The most common sources are:
- OJ and breakfast cereal
- Cow’s Milk, 1 cup contains around 120 IU
- Non-dairy milk, milk alternatives *variable levels, from 11-145 IU
- Dairy products
Supplements
Nutritional Vitamin D supplements can be obtained over the counter, and by prescription when higher doses are needed. There are different sources and types of Vitamin D worth knowing about.
Different Types of Vitamin D
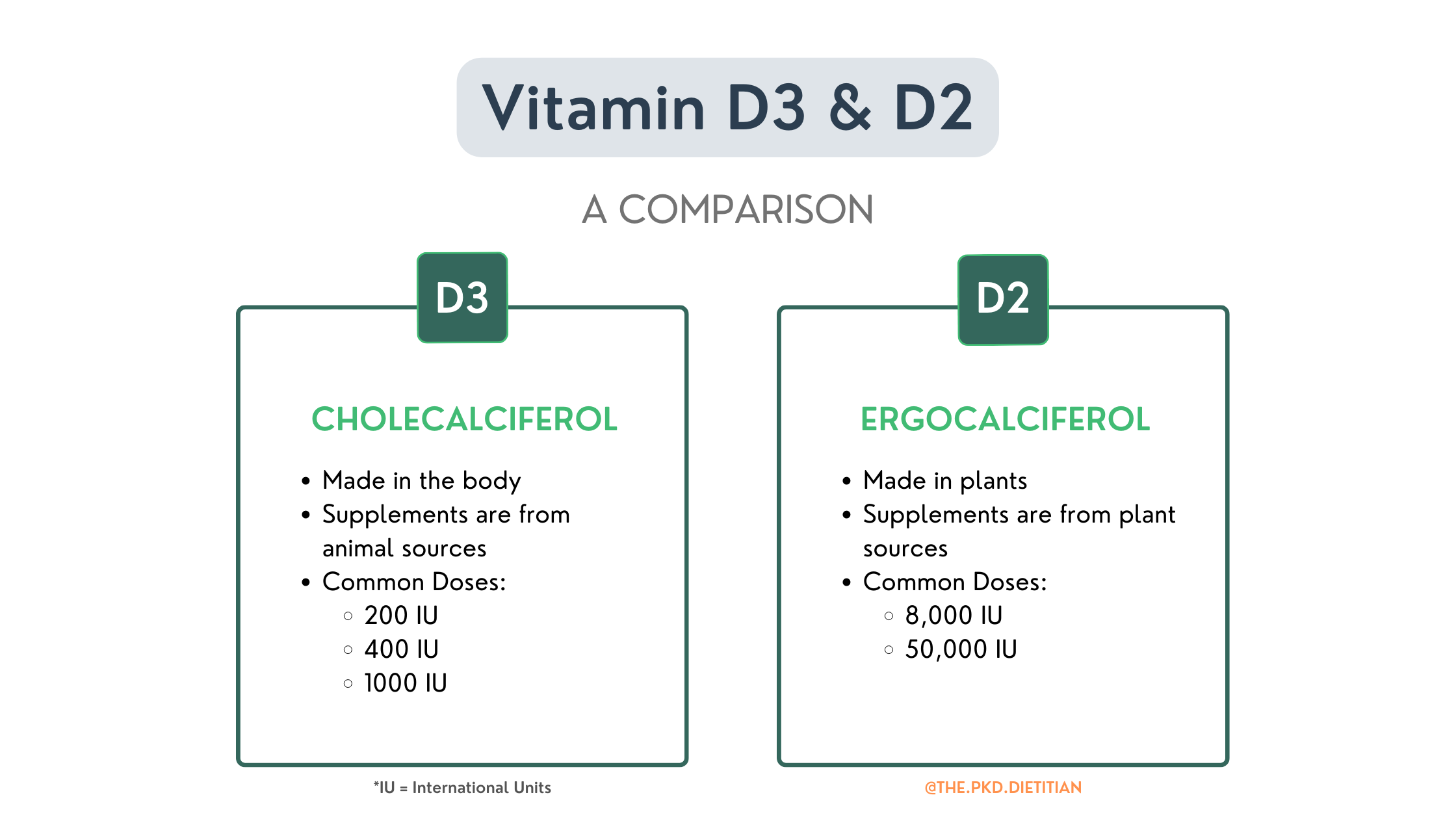
There are two main forms of Vitamin D found in food and supplements, Vitamin D3 (cholecalciferol) and Vitamin D2 (ergocalciferol). Both forms are well absorbed in the body and can help increase the amount of stored and circulating Vitamin D.
Vitamin D3 supplements are made naturally from animal sources while Vitamin D2 is synthetically sourced from plants, primarily mushrooms. You will find both forms of Vitamin D supplements over-the-counter (OTC), but higher dose versions for Vitamin D2 are prescription only.
When supplementing for a deficiency, Vitamin D3 has been shown to be more effective at increasing levels in the body. (16, 17) It's worth noting that Vitamin D isn’t just found as a solo supplement but is frequently included in many multivitamins.
Vitamin D in the Body
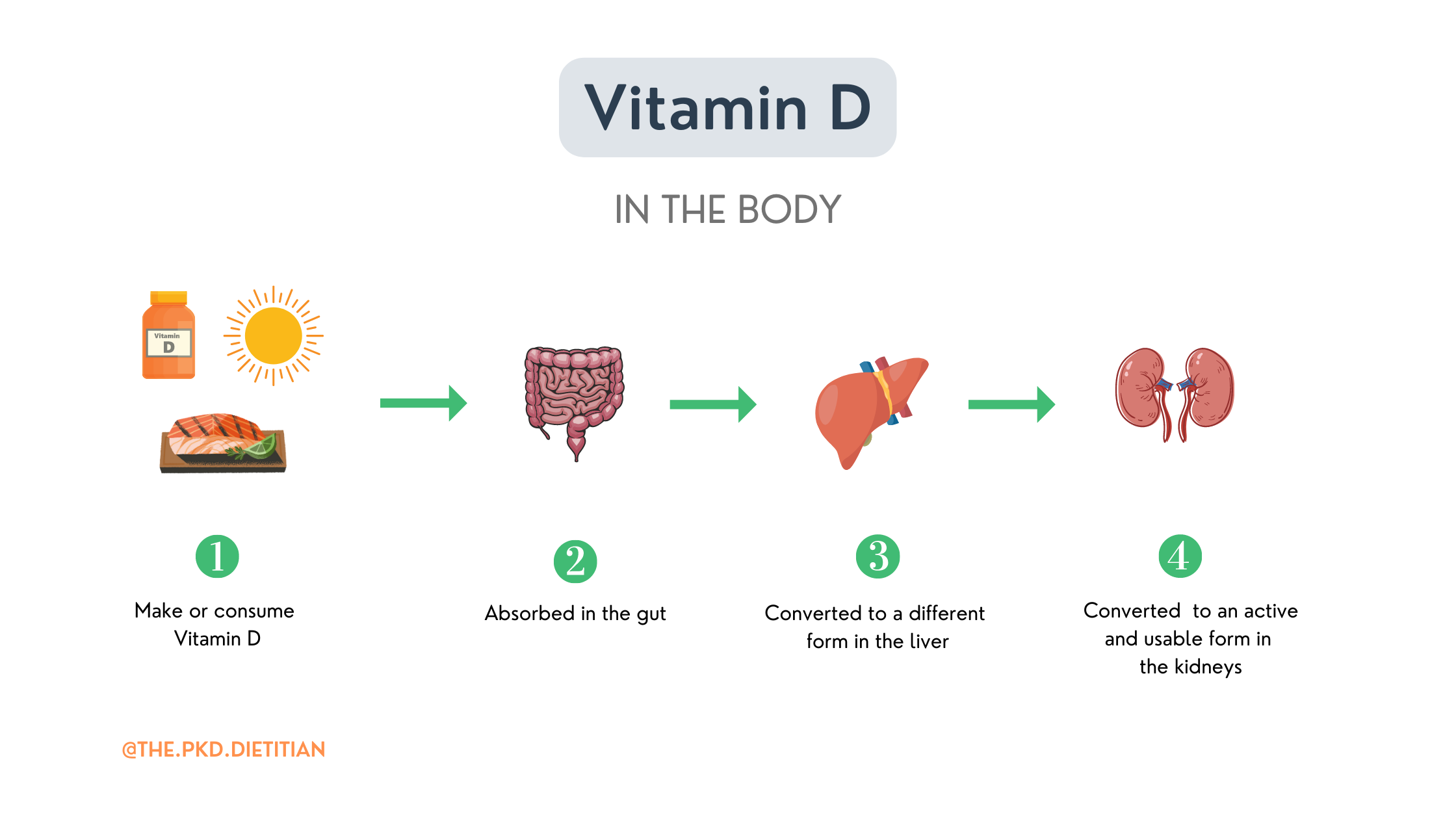
In our bodies, both forms of Vitamin D are metabolized to an “active form” of Vitamin D in the liver. Yes, it's true that D2 takes some extra steps to get there but it eventually does.
After you consume Vitamin D it's absorbed in your gut and transported to your liver. This will get a little "sciencey" but stick with me. In the liver, Vitamin D is converted to a different structural form called calcidiol (Vitamin D 25-hydroxyvitamin D). You may see it written as 25(OH) on your labs. Calcidiol is considered a “pre-hormone” form of Vitamin D.
This form of vitamin D, calcidiol, is the body’s storage form of Vitamin D and is also what is measured when you get levels tested. Levels of calcidiol directly reflect the body’s stores of Vitamin D.
But the conversion of Vitamin D doesn’t stop there!
After the liver, that storage form of Vitamin D is transported to the kidneys where kidney enzymes help convert it to what is considered an active form of Vitamin D. A form that can be used by the body. The end result of this whole process is a hormone called calcitriol. Yes, you read that correctly, the form of Vitamin D our body actually uses functions like a hormone.
Are you picking up on the importance of having enough Vitamin D coming in to convert to the active form, but also the importance of the kidneys in that final step?
Here is the flow of Vitamin D from the sun, food, and supplements:
I want to take a moment and clarify some confusion around Vitamin D I run into. If your MD has prescribed Calcitriol, this is the hormonal form of Vitamin D, not a supplemental form. Calcitriol is prescribed when there is already an imbalance in your bone health and your kidneys aren’t doing their job of responding to help correct it.
Calcitriol will not improve your Vitamin D status or levels, it is the very end result of Vitamin D conversion. Starting calcitriol does not mean automatically stopping supplemental Vitamin D. Please review your bone health-related meds and supplements with your MD and Dietitian before making any changes.
The Kidney Connection
Let’s look at the last piece of this process, the kidney connection! Your kidneys play an important role in converting Vitamin D into its active form which the body can use.
Kidney enzymes convert the calcidiol form of Vitamin D into an active form, calcitriol. Those two are pretty easy to get confused! The active form, calcitriol, functions like a hormone helping to regulate calcium and phosphorus in the body, and bone health balance.
Any kidney injury or altered function, like with PKD or CKD, is itself a risk factor for Vitamin D deficiency. Deficiencies are found in all stages of kidney disease and become more common with a reduced GFR, a reduced kidney function.(18,19)
Since the kidneys are responsible for turning inactive Vitamin D into its active form in the body, any injury or impaired function can alter this process. Conversion to that active form can be suppressed. Injured, or kidneys with lower function often have decreased ability to convert vitamin D into its active form.(20)
Any form of chronic kidney disease (CKD), including PKD, can result in changes to, and the balance between, Vitamin D, calcium, and phosphorus.(21) This results from several mechanisms that affect the kidneys, including a decrease in the enzymes needed for the conversion of Vitamin D. Because of this, Vitamin D levels tend to decline gradually.(22)
Some folks with CKD spill protein into their urine, and many folks with PKD do. This is a sign of kidney damage. When the levels of protein spilling into urine get high, called proteinuria, it can also affect Vitamin D status too.
High levels of protein in the urine can promote a Vitamin D deficiency. Different forms of Vitamin D bind to proteins in the body and are lost when proteins spill into the urine.(23)
That brings us to a bit more specifics when it comes to PKD and Vitamin D.
The PKD Connection
In addition to everything just reviewed, there are two areas I want to highlight that are important for Polycystic Kidney Disease (PKD):
-
Having any kidney injury, which includes PKD, regardless of kidney function puts you at a higher risk for Vitamin D deficiency and altered bone balance. With PKD this can start earlier even with a "normal" GFR.
-
If we wait to look at Vitamin D levels and status until there is a decline in kidney function, this is much too late in my opinion. There already could, and often are, imbalances, insufficiencies, and deficiencies.
With PKD bone health, and Vitamin D status and monitoring should be part of a proactive nutrition plan. This needs to become best practice and part of PKD's standard of care.
What Does The Science Say?
There have been some smaller studies specific to PKD looking at Vitamin D status.
Research suggests that low having low levels of Vitamin D is associated with a larger kidney size, the TKV.(24) This hasn't been shown to be a cause-and-effect relationship but more of an association.(25)
There is also a known link between Vitamin D deficiency and HTN.(26) A deficiency is believed to potentially contribute to the activation of the pathways that drive higher blood pressure and cyst cell growth.(27, 28) We want to avoid both complications with PKD.
Animal studies have shown a long-term vitamin D deficiency, with PKD, negatively affected BP, heart health, and even impacted kidney function.(29)
It is not a stretch to conclude that being deficient in Vitamin D has the potential to negatively affect blood pressure regulation and have an impact on kidney health and PKD progression. Long-term studies are needed for sure. The thing is, fixing a deficiency, especially if caught early can be easy.
Vitamin D is important for PKD health beyond bone health, it could potentially help with blog pressure management and may act as an inflammation regulator. Both of which are known to be directly involved with the progression of ADPKD.(30,31)
Recommended Intake
Recommendations for the daily intake of Vitamin D don’t differ if you have altered kidney function, chronic kidney disease (CKD), or polycystic kidney disease (PKD).
Current Guidelines
Current guidelines regarding Vitamin D and kidney health are the same ones that are recommended for everyone, the “general population”.
They don’t take into consideration any altered kidney function. This is a heavily debated topic in the kidney world. Studies are ongoing looking at questions like how much is enough? What lab level is good?
It was in first in the 1940s that recommendations for Vitamin D were first made. The amount recommended was 400 IU daily, this level was to prevent rickets in infants. This recommended intake is primarily to prevent disease caused by deficiency and not for optimal health. There is a big difference between the two if you ask me.
Only a minor increase in recommended intake has been made since then.
The current daily recommended dietary allowances (RDA) are:
-
400 IU (10 mcg) up to 1-year-old
-
600 IU (15 mcg) for everyone 1-70 years old
-
800 IU (20 mcg) for adults greater than 70 years old
What is a Deficiency?
There are also different opinions as to what counts as a Vitamin D deficiency versus an insufficiency. A general consensus is that a serum Vitamin D less than 20 ng/mol is deficient and that a level < 30 ng/mol is insufficient. Lower levels are associated with osteoporosis, bone imbalances, and inadequate intake.(32,33,34)
Regarding the kidneys, a serum Vitamin D level < 30 ng/mol is associated with a higher risk of secondary hyperparathyroidism (SHPT).
What Causes a Deficiency?
In general, there are two main causes of Vitamin D Deficiency.(36)
-
Not getting enough vitamin D from diet, supplements, or through sunlight
-
Not absorbing Vitamin D properly.
How To Test Vitamin D Levels
Your provider can order a blood test to measure Vitamin D serum levels. There are two types of tests that they might order, but the most common is the 25-hydroxyvitamin D, known as 25(OH)D for short.
Testing Guidelines
KDIGO (Kidney Disease Improving Global Outcomes) recommends testing monitoring of Vitamin D should start with CKD3, that is with a GFR < 60. Based on what that baseline level is and what trends show, Vitamin D should be "assessed and monitored" every 6-12 months.(37)
KDIGO states “It is important to take into account trends, rather than single values”. At a minimum, Vitamin D levels need to be checked yearly.
The National Kidney Foundation and KDOQI (Kidney Disease Outcomes Quality Initiative) has a slightly different approach to its clinical guidelines. They recommend, with CKD3 and CKD4 to first check the Parathyroid Hormone (PTH) level. If it's within a normal range, then recheck the PTH annually.
These are recommendations specifically for CKD and PKD is lumped in with them. We know kidney damage happens in PKD because of cyst growth and this is occurring well before any decline in estimated GFR. I look forward to more proactive, and standardized recommendations for Polycystic Kidney Disease around assessment of Vitamin D and bone health status.
My Thoughts and Practices
As a Renal Dietitian who specialized in PKD, I have all my clients request to have Vitamin D checked. Based on their level, kidney function, other bone health labs, diet, and supplements we set up a proactive plan to replete their stores, if necessary, and for long-term monitoring.
A Vitamin D deficiency, or insufficiency, is generally pretty easy to fix. The problem is that levels aren't getting tested early enough within the PKD Community therefore no intervention or treatment is being put in place.
Toxicity
Is it possible to get too much Vitamin D? YES.
Let me explain. You won’t and can’t get too much Vitamin D from sun exposure or from dietary intake. This happens only through supplementation.
How much is too much?
Getting enough vitamin D is important for your health, but taking too much can lead to toxicity. The risk of toxicity is associated with supplements.
Vitamin D is fat-soluble and can be stored for longer periods of time in body fat. Because of this, excess supplementation creates a risk for toxicity. Especially long-term supplementation without monitoring serum levels.
Megadosing
According to the National Institute of Health (NIH), a megadose of vitamin D is 6000 IU and greater. There are maintenance doses of Vitamin D and there are Therapeutic doses of Vitamin D. What benefits you can change over time. It is best to review your level and intake with your Healthcare team to determine your needs.
Avoid megadosing, which can put you at risk of toxicity. But also at a greater risk for elevated calcium levels, kidney stones, and gut issues.
Vitamin D enhances calcium absorption. That's generally a good thing, we need calcium for strong bones. But with very high Vitamin D doses, only seen with supplementation, it can go too far and result in high calcium blood levels which can negatively impact your muscle and heart function. If you have ever heard the term calcification, that's what I am referring to here. Calcification is good in your bones, not in your soft tissues and organs.(38)
Long-term “megadosing”, lead to calcification of some soft tissue, and heart vessels and cause further kidney damage.
Your Next Steps
Let’s get into what to do for your Proactive PKD Plan for Vitamin D.
-
Regardless of what your kidney function is, if you have never had your Vitamin D tested, get it done. You want a baseline level. Make a plan to at a minimum get it checked yearly. This way you can know your number, know your trends, and easily put interventions in place if your levels are less than ideal.
-
If you have had your vitamin D checked, go look at how long ago it was. If it was greater than a year, ask to get it retested with your next labs, and at least yearly after that.
-
Your provider can order a blood test to measure your levels of vitamin D.
-
If needed, your Doctor and dietitian can recommend your appropriate level of supplementation.
If you are a podcast fan, check out the episode Vitamin D and PKD: How To Supplement Safely on the PKD Dietitian Podcast for more on Vitamin D and PKD.
If you want to dive even deeper into your bone health and Proactive PKD Nutrition, and get expert recommendations and support, check out your options for working together.
In health, bone health that is!
Diana, The PKD Dietitian


