Kidney Stones & PKD, Can Nutrition Help?
Oct 25, 2022Diet and lifestyle both factor into the risk of forming a kidney stone. With PKD it's important to consider both for preventing a first, or even a second stone from forming.
The good news is that dietary changes that reduce stone formation risk align with dietary changes to support PKD health and promote slower progression.
First, let’s identify patterns that create an environment for oxalate and uric acid stones, the two most common stones formed with PKD.
Second, let's flip those risk factors into my 6 Dietary Choices & Changes you can make right now that are healthy for PKD and go a long way toward stone prevention.
We are going to Wrap Up with a look at what to do if you have had a stone, make sure to snag my freebie roadmap that walks you through exactly what to do!
Dietary Patterns and Kidney Stones
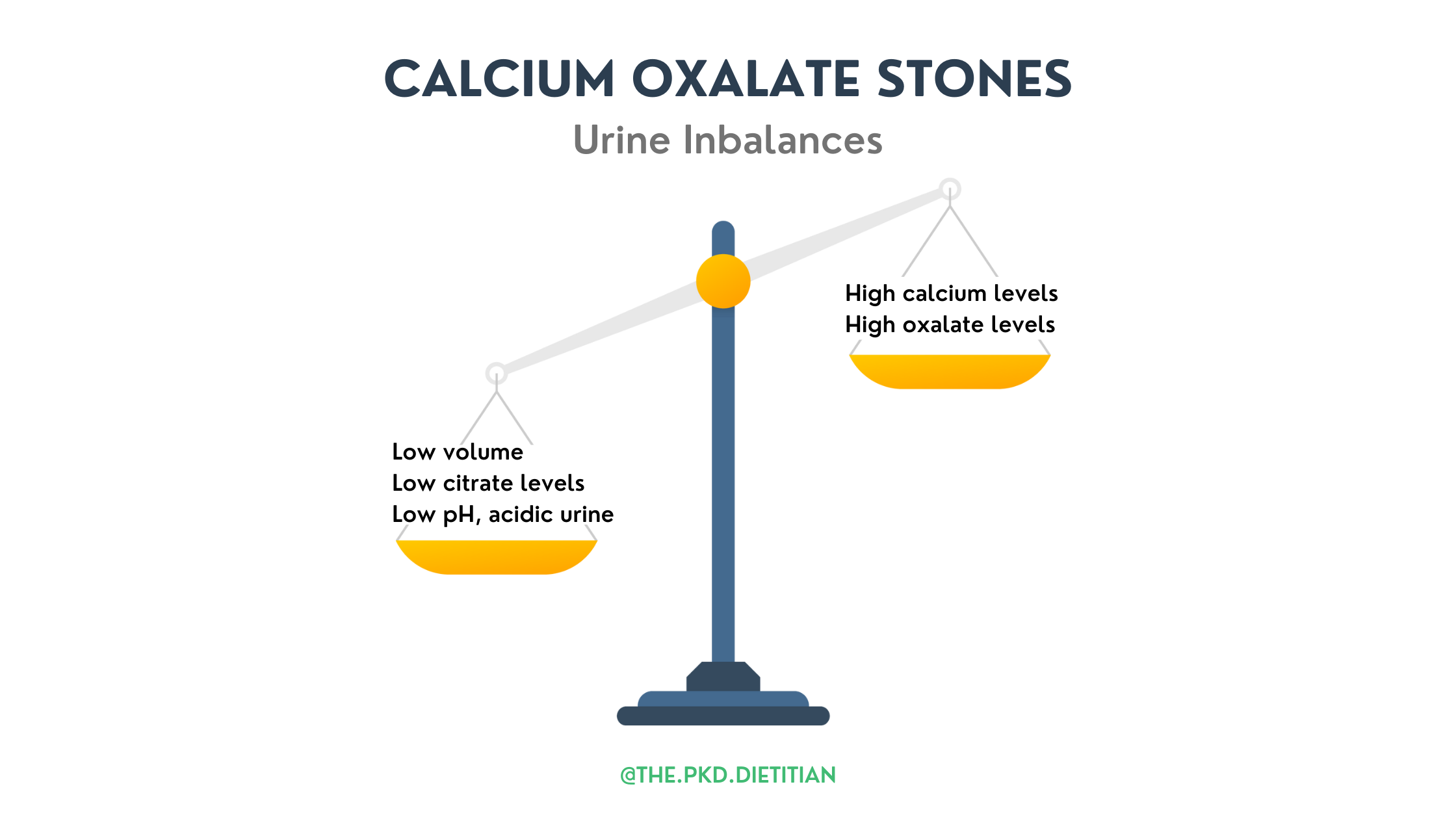
Risk factors, when it comes to diet and kidney stones, are well known! Common risk factors all contribute to urine imbalances and an environment that is conducive to stone formation. (1)
Common Risk Factors for Kidney Stones:
1. Poor Hydration
Overall fluid intake, especially water, is important not only for PKD but also for stone prevention. Water helps increase urine output and keeps things “moving” through the kidneys and urinary tract. Good hydration also helps dilute particles in urine that like to come together and form crystals. Essentially it reduces urine saturation of minerals! A high saturation increases the risk of stone formation. (2)
2. High Sodium Intake
A diet that is heavy in sodium, much like the Standard American Diet, is a stone risk factor. Not only does it reduce urine output, but a high sodium intake pulls calcium from the bones and dumps it into the urine. A heavy sodium intake competes with calcium for absorption, also contributing to more calcium in the urine.
In addition, heavy sodium intake decreases urinary citrate levels. (3) Remember, when it comes to urine, citrate is good to have and calcium isn't!
3. Heavy Animal Meat Intake
Heavy animal protein intake, specifically animal meat, is an independent risk factor for stones. Animal meat generates a large acid load during digestion. Not only does this work the kidneys harder to have to balance, but it also reduces urinary pH creating more acidic urine. Animal meat is purine-rich, which leads to greater uric acid production during its breakdown in the body. (4) Heavy intake of animal meat is also associated with increased calcium in the urine and lower citrate levels. (5) A perfect quiet storm for stone formation.
4. Low Fruit and Vegetable Intake
A diet with limited fruits and vegetables lacks stone-preventing agents that are prevalent in produce. Fruits and vegetables are rich in potassium, magnesium, citrate, and are alkali/base producing. Citrate helps prevent stone formation by blocking oxalate and calcium from joining and helps increase acidic urine’s pH. Diets low in fresh produce are often heavy in processed foods that are loaded with added salt and sugar, both of which are associated with increased stone formation risk. (6)
5. Poor Dietary Calcium Intake
Not meeting dietary calcium needs is a risk factor for calcium oxalate stone formation. Calcium, in the gut, binds with oxalate and prevents it from being reabsorbed and crystals from forming. Because calcium binds with oxalate in the gut and hinders its absorption, oxalate is more readily absorbed when dietary calcium intake is low. Calcium in the urine isn't caused by higher dietary intake. (7)
6. Heavy Oxalate Load
A high intake of oxalate-rich foods is associated with higher urine concentrations of oxalate. The best way to manage oxalate load is to control the consumption, and frequency, of very high oxalate items but also to ensure adequate calcium intake. (8, 9)
7. Certain Supplements
Certain supplements are associated with an increased risk for kidney stone formation. High levels of vitamin C supplementation, > 500 mg per day, are associated with increased stone risk. (10) Why? Because a waste product of supplemental Vitamin C is oxalate which leads to increased urinary levels. (11) Collagen, which is a protein supplement, also produces oxalate as waste. Of note, excess supplementation of Calcium, especially taken between meals, can increase the incidence of stone formation also. (12, 13)
Medical History and Kidney Stone Risk
Certain medical conditions are associated with an increased risk and occurrence of kidney stones. (14,15) If you have a diagnosis of one, or more, of the following it is worth a discussion with your Doctor about stone prevention, any other risk you may have, and perhaps further testing to get ahead of a potential stone. (16) This can include both blood and urine testing!
- Gout
- Obesity
- Irritable bowel syndrome (IBS)
- Chronic Diarrhea
- Hyperparathyroidism
- History of bariatric surgery
- Family History of Stones
- Hypertension (HTN)
For more on Polycystic Kidney Disease, what kidney stones are and how they form, plus the driving factors associated with PKD and kidney stones occurrence, check out Part 1. of my two-part stone series. The two most commonly occurring stones with PKD are calcium oxalate and uric acid stones. (17) Specific urine imbalances are associated with each. (18, 19, 20)

Diet and Stone Prevention
What Can You Do?
There are dietary patterns and choices that are important for preventing kidney stones. (21) This is the good part, you can flip those known risk factors around into dietary action, and perhaps changes, for you! All positive for PKD health. Check out my top 6 Dietary Choices & Changes for PKD health and stone prevention.
1. Good Hydration Habits
A good goal, with water being best, is 3-4 liters of fluid a day! Not only is this positive for PKD but leads to an increased urine volume and dilutes urine’s minerals and promoters of stones. Good hydration is the #1 way to help prevent stones! (22)
2. Keep Sodium Intake Low
The easiest way to do this is to cut out processed food, it's generally a sodium bomb. First, look at how much you are actually consuming then set a goal to reduce your intake. Not sure of a good goal? Ask your Dietitian, or MD, for your best goal. For PKD, a good range is 1500-2000 mg/day of sodium per day.
3. Reduce Animal Meat Intake
Animal meat, rich in purines, is the biggest dietary contributor to uric acid waste. Yes, that same uric acid that forms kidney stones and contributes to Gout. Reducing, or eliminating, animal meat decreases uric acid production and helps to achieve a better urinary balance of citrate and neutral pH. Animal meat protein is pretty harsh on the kidneys but also, in excess for individual needs, detrimental to PKD.
The “general” recommendation for PKD is based on CKD recommendations of 0.8-1.0 grams of protein per kg of body weight. This 100% should be individualized to your needs. PKD isn’t CKD and the are other factors specific to you that come into play.
It is best to work with your Dietitian or Doctor to explore your individualized protein needs. (23)
4. Increase Fruits and Vegetables
Not only are fruits & veggies packed with fiber, phytonutrients, and delicious, they also contribute stone-preventing properties. The magnesium, calcium, citrate, and potassium in fruits and vegetables all help to prevent stone formation. Fruits & Veggies are also alkaline/base producing so don't contribute to lower urine pH, acidic urine.
Skip the very high oxalate load fruits & veggies like spinach, almonds, dates, and rhubarb.
Include good sources of citric acid including lemons, limes, and other citrus as able. Around 4 oz of lemon or lime juice, a day has been shown to increase urinary citrate levels.
5. Include Calcium Rich Dietary Sources
Reduce urine calcium and support healthy bones by meeting your needs, as able, with dietary intake. The recommended calcium intake is between 1000-1200 mg/day. (24) Dairy is a great source of calcium, ensure it doesn't have added sugar! Veggies like bok choy, broccoli, kale, and even Brussels sprouts are also good caused of calcium. If you aren't able to meet your calcium needs with diet, talk to your Dietitian or MD about safe supplementation.
6. Skip Certain Supplements
Skip collagen and high doses of Vitamin C supplements. I tell clients to be wary of any supplement with > 250 mg of supplemental Vitamin C. The key here is SUPPLEMENTAL, Vitamin C from food is a good thing and won't lead to added oxalate waste.
Please review any supplements you are interested in taking or are taking, with your Dietitian and Doctor.
Had A Stone? 4 Steps To Take
Knowing the type of stone formed is essential for treatment, prevention, and identifying the most impactful dietary changes. (25) You have to address the stone’s cause! This lets you take target steps to prevent a recurrence.
Stone analysis and a 24-hour urine identify the type of stone formed and the urine environment and chemistries that contributed. This helps individualize your nutritional and potentially medical treatments. A 24-hour urine can show areas of diet to focus on like fluid, protein, calcium, oxalates, or sodium intake just to name a few.
Have you had a stone or been told there are stones showing up on your scan?
Grab my freebie guide PKD & Kidney Stones Roadmap To Dietary Prevention. It walks you through 4 steps to take and what to do!
Happy & Healthy Eating,
Diana, The PKDietitian

